Diet and Osteoarthritis
February 4, 2020
Once an individual understands that the osteoarthritis (OA) in their knees is not solely from wear and tear, and that, in fact, ongoing inflammation is at the core of the pathology, the question becomes (hopefully) “What can I do to stop (or even reverse) the damage?”
One option…
…is knee joint replacement surgery which, when successful and assuming you survive, can certainly eliminate some of the sources (subchondral bone, joint capsule, menisci, articular cartilage) of inflammation and pain. There is however that one inconvenient truth: Almost 1 in 200 folks who undergo this surgery will be dead in 90 days. Of the 199 who survive, roughly 40 are not going to be happy with the result. As Clint Eastwood once asked a bad guy staring down the barrel of his canon like pistol: Do you feel lucky?
A far better option…
…that won’t kill you is changing the way you eat. One of my medical heroes is Dr. Michael Gregor of www.Nutritionfacts.org
fame. He has a tremendous new book out: How Not to Diet. In the book he describes obesity as the “main modifiable risk factor” for osteoarthritis. He cites one study that showed 20 lbs. of weight loss to be a reasonable alternative to knee replacement surgery!
As we have discussed, it is not just wear and tear from carrying excessive weight that cause osteoarthritis, else why would OA show up in our hands. The inflammatory qualities of our American diet lead to obesity and then the additional pro‐inflammatory molecules generated by the excess fat drive the osteoarthritic process. PS: For a little extra kick‐start: An inflammatory diet has been shown to increase cancer risk by 75%
What’s great is you don’t have to reach your senior year weight to reap the benefits of an anti‐ inflammatory diet – you just have to start the process. Within days of going to a plant‐based, high fiber, low saturated fat (meat, dairy, processed foods), inflammatory markers like hsCRP begin dropping to normal levels and you may notice yourself feeling better, hurting less, thinking more clearly.
Combined with regenerative treatments at Atlanta Osteoarthritis Clinic, …
…I am confident that changing to a plant‐based diet (and possibly adding some useful supplements) will change the arc of your health and life. YOU CAN DO THIS!
There is so much to more learn about this topic and the knowledge you will gain is so empowering. I strongly recommend following Dr. Gregor at www.nutritionfacts.org
as well as reading his How Not to Diet. Search “anti‐inflammatory foods”. Signing up to his web page is free and all proceeds from his books go to charities.

1. Offloading Braces: Your Knee’s Knight in Shining Armor Offloading braces, also known as unloader braces, are not your ordinary knee supports. These aren't just about keeping your knee in place; they're about shifting the load away from the part of your knee that's crying out for help. Imagine your knee as a teeter-totter that’s stuck in the wrong position. Offloading braces come in to adjust that balance, relieving pain and improving function. These braces work by applying force to the thigh bone, pushing it away from the knee area that’s worn down or damaged. It's like having a gentle but firm hand guiding your knee back to its happy place, where it doesn’t feel every step is a chore. 2. The Science of Relief: How Offloading Braces Work Their Magic The beauty of offloading braces lies in their ability to redistribute weight inside the knee joint. This redistribution can significantly reduce the load on the damaged part of the joint, decrease pain, and increase mobility. Think of it as redistributing the weight in a overloaded backpack so it’s easier to carry. Studies have shown that using an offloading brace can lead to a reduction in pain and an improvement in daily activities for people with knee osteoarthritis. It’s like turning down the difficulty level on your daily life settings, making everything a bit easier to manage. 3. Who Can Benefit? Unlocking the Potential of Offloading Braces Offloading braces are particularly beneficial for individuals who have knee osteoarthritis primarily on one side of the knee. They’re a game-changer for those who want to: Stay Active: Ideal for people who aren’t ready to give up their walks in the park or trips to the mall. Delay Surgery: Perfect for those who are looking for non-surgical options to manage their knee pain. Enhance Other Treatments: Great as a companion to medications, physical therapy, or injections, adding an extra layer of support and pain relief. 4. Embracing a New Lifestyle with Offloading Braces Wearing an offloading brace can be a big step towards reclaiming the active lifestyle you love. It’s like hiring a personal assistant for your knee—one that’s dedicated to making sure you can keep doing what you enjoy without the extra pain. It's important to remember that while offloading braces can be incredibly effective, they work best as part of a comprehensive approach to knee health, including exercise, proper nutrition, and medical care as needed. Final Thoughts: Step into the Future with Confidence If you're battling with knee osteoarthritis and looking for a way to ease the burden, consider giving offloading braces a try. They might just be the support your knees need to help you move through life with more ease and less pain. So, strap in and brace yourself for a more comfortable journey on those two amazing legs of yours. Here’s to moving forward, one well-supported step at a time! Cheers to better mobility and a brighter, less painful future!
Ladies and gentlemen, fasten your seatbelts and recline your seats because we’re about to take a dive into the future of knee pain relief. Imagine if there was a way to literally lubricate your joints like a well-oiled machine—well, guess what? There is, and it’s called viscosupplementation. And when paired with the wizardry of a fluoroscope for guidance, it’s like having GPS for your joints! 1. Viscosupplementation: The Lube Job Your Knees Crave First off, let’s unpack viscosupplementation. This isn’t just any treatment; it’s like a spa day for your knees. Here’s the scoop: Viscosupplementation involves injecting hyaluronic acid directly into the knee joint. Why hyaluronic acid? It’s a natural part of your joint fluid—its job is to keep things moving smoothly by acting as a lubricant and shock absorber. Think of it as premium motor oil, but for your knees! This gooey goodness can help reduce pain, improve mobility, and generally make your knees feel younger than a spring chicken at a disco. 2. Enter the Fluoroscope: Your Joint's New Best Friend Now, let’s add some high-tech flair with the fluoroscope. This isn't your grandma’s X-ray; it’s a real-time imaging technology that allows doctors to see your joints in action during the injection. It's like having a live satellite feed to ensure the hyaluronic acid hits the sweet spot with the precision of a master archer. Why is this important? Well, imagine trying to pour syrup on a pancake in the dark. Messy, right? The fluoroscope lights up your joints from the inside, making sure every drop of hyaluronic acid is perfectly placed for maximum effectiveness. No mess, no fuss, just smooth sliding. 3. The Dynamic Duo: How They Work Together Pairing viscosupplementation with fluoroscopic guidance is like having Batman and Robin in your medical team. The fluoroscope guides the way, ensuring the hyaluronic acid is delivered exactly where it’s needed most. This dynamic duo can: A. Reduce Pain: Like turning down the volume on your knee’s scream-o-meter. B. Increase Mobility: Get ready to boogie at weddings again without thinking about your knees! C. Extend Joint Health: Think of it as adding miles to your knees' odometers. 4. What the Science Says: A Peek at the Research Clinical studies have shown that when viscosupplementation is administered with the accuracy of a fluoroscope, patients often experience a significant improvement in knee pain and function. It’s like hitting a bullseye in the dart game of joint treatments—highly satisfying and impressively effective. 5. Who Should Consider This Treatment? If you’ve been wrestling with knee osteoarthritis and traditional methods like medications and physical therapy are like bringing a knife to a gunfight, then viscosupplementation might be your howitzer. It’s particularly suited for those who are looking for an alternative to surgery or for whom other treatments have done about as much as a band-aid on a broken leg. Final Thoughts: Glide into a New Chapter of Knee Health So, if you're dreaming of days where your knees might feel like they’ve sipped from the Fountain of Youth, viscosupplementation with fluoroscopic guidance could be your ticket to a smoother tomorrow. Talk to your doctor about whether this futuristic fix can put the spring back in your step and the joy back in your "joints!" Here’s to less pain, more gain, and a high-tech way to keep those knees in the groove! Cheers to advanced medical magic and the wonders of science!

Discover how the Mediterranean diet can ease joint pain and enhance overall joint health. This guide explores the anti-inflammatory benefits of Mediterranean foods like olive oil, fish, and whole grains. Learn tasty recipes and dietary tips that not only delight your taste buds but also soothe your joints.

When considering supplements for any medical condition, patients and recommending physicians should always keep safety as the first priority. In many cases, there are certain side effects and drug interactions that need to be considered. These are easy to research online at locations such as https://www.webmd.com/interaction‐checker/default.htm . Those on blood thinners, chemotherapy drugs, those with kidney disease, those on multiple medications metabolized by the liver, females in their child‐bearing years all need to be wary of starting any supplement without discussion with their primary care physician. If you are a patient of Atlanta Osteoarthritis Clinic, it can be presumed that your joint issues are a major health issue and there is a certain urgency for pain relief and improved function and mobility. The tendency is to want to try every newly advertised and promising supplement that comes along. I have certainly been there! Keep in mind however that the marketing of supplements is big business and the truth can and will be stretched to separate you from your dollars. Also, realize that because many supplements, particularly common herbs, cannot be patented, so there is not much financial incentive to engage in expensive human studies for something like ginger for example. All the good things you have heard about a particular supplement may be based entirely on a test done in a tube or petri dish (in vitro) or animal studies. That doesn’t mean the supplement is necessarily any less helpful, just that it might require a bigger leap of faith. Personally, I have very strong favorable convictions about the ability of certain substances to enhance the results of our injection therapies and further reduce your suffering related to osteoarthritis. Some of these substances are also at the forefront of anti‐aging research. In future postings, I will discuss those that I believe are most likely to have the most positive impact.

Some very smart scientists found that supplementing the precious joint fluid to the osteoarthritic knees of lab animals seemed to give these critters a bit more bounce in their step. After going through the usual trials, hyaluronic acid (HA) was approved for use in humans. Viscosupplementation is the process of injecting hyaluronate into a joint, which is typically in a weight bearing joint, generally the knee. What is Hyaluronic acid (HA)? It has many names: Durolane, Hyaluronan, Hyaluronate Sodium, Hyaluronic Acid, Hylan G‐F 20, Hylan Polymers, Sodium Hyaluronate – confusing, no? We’ll stick with HA here. HA is a gel like substance we have within our joints. In the knees, it acts as both lubricant and shock absorber to protect the cartilage. Incredibly, with slower movements it tends to remain in a thickened state for maximum protection against friction, while when the action is faster and more furious, it will tend to thin out to protect against impact/compression forces. Not a One‐Trick‐Pony ‐ It’s an anti‐inflammatory: Pro‐inflammatory molecules (bad guys) are released by cells of our joint lining (synovium) and our cartilage when HA levels are low. This happens as the joint ages and osteoarthritis is a result. Injecting HA back into the joint suppresses release of the inflammatory substances and stimulates release of anti‐inflammatory factors from those same cells. ‐ It stimulates our own HA production: HA is a signaling molecule to the receptors of various area cells, provoking the production of not just our own (endogenous) HA, but also additional extracellular matrix proteins involved in cartilage building. ‐ It’s analgesic (pain relieving): The only joint tissue that doesn’t cause knee pain is the articular cartilage. Every other tissue involved has pain receptors and as many know, the pain can be severe and persistent. HA has been shown in to be every bit as effective and often more effective than anti‐ inflammatory drugs (NSAIDs) and cortisone injections…without all the side effects of the latter. ‐ It’s regenerative: HA accumulates in the articular cartilage and subchondral bone. Healthy levels preserve cartilage volume and there is some evidence that it may regenerate lost cartilage volume. ‐ It’s a surgical alternative: A study of nearly 1200 severely (grade 4) osteoarthritic knees were deemed (doomed?) ready for total knee arthroplasty. They received a protocol of viscosupplementation. At nearly 4 years, 75% of those knees had still not required surgery! Viscosupplementation is the cornerstone of our regenerative knee program at AOC. A healthy knee has about 2 milliliters of joint fluid and 5 to 8 milligrams of hyaluronate. As years pass, we lose volume and HA content. At AOC, our protocol combines the best Hyaluronate products available, injection techniques that provide the highest rate of correct HA placement, and vital pre‐ and post‐injection care and ancillary therapies. The goal: Decreased pain; Improved joint function; As many years in your natural knees as possible. LRK
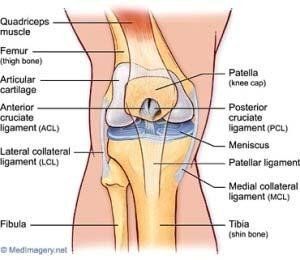
When I was home on Christmas break during my first year of medical school, we were visited by my uncle Ed, an ENT surgeon from Portland, Oregon. We were talking about the daunting upcoming semester schedule, which included Gross Anatomy. I’ve never forgotten what he said: “Lary, throughout your career, anatomy will serve you well.” He was correct of course and I think some anatomical knowledge serves all of us well. So, without further ado here are a few pearls about the engineering miracle that is your knee.

One of the promising therapies in regenerative medicine is PRP or platelet rich plasma. This particular therapy has been gaining quite a bit of media attention for its popularity and frequent application by elite athletes such as tennis superstar Rafael Nadal, golfing legend Tiger Woods, soccer champion Cristiano Ronaldo, and countless others. While it is probably more frequently utilized in chronic tendon and ligament issues, the logic of its application to osteoarthritis of the knees and elsewhere is also compelling. There have been studies showing “significant improvement” when PRP is injected into the osteoarthritic knee, particularly those with grade 2 (relatively early) degeneration. More than the limited studies and the endorsement of star athletes, PRP therapy is a promising option for osteoarthritis because of the known physio‐chemical responses to the components of PRP. So, what is PRP? In short, it is a concentration of your own platelets and 100s of various natural protein factors essential to tissue growth and healing. It is produced by spinning your own blood sample down in a centrifuge, which separates away the red and white blood cells, leaving the plasma portion containing the your platelets and tissue growth factors for injection. How does it work? Platelets are interesting. They are lacking components to be complete cells but they do fortunately contain what are known as alpha granules . Once injected into the damaged area, these granules release hundreds of proteins. These growth factors activate the cells of your cartilage to promote the creation of new cartilage matrix. PRP also has the ability to increase stem cell and chondrocyte activity. Additionally, platelets seem to slow the process of cartilage degeneration in osteoarthritic joints. Who is it for? PRP is most suited to chronic joint, tendon, and ligament conditions that haven’t responded to traditional healing methods such as rest, physical therapy, protective bracing, etc. It may be helpful when there is some urgency in regards to recovery time. Specifically, regarding the osteoarthritic knee, I would suggest that our therapy protocol of hyaluronate injections be utilized first before proceeding to therapies like PRP and stem cell injections. Yes, PRP can be used together with stem cell treatment. It is important to know that medical insurance does not cover the cost of either PRP or stem cell treatment, but our patient care coordinator will be very happy to discuss the cost and payment options with our patients. LRK

What an important word to be familiar with. It is a very clever combination of the words “inflammation” and “aging”; 2 words that, as Forrest Gump might say, “..go together lie peas and carrots.” Why is it an important concept for our clients at Atlanta Osteoarthritis Clinic (AOC) to understand? Because you are investing your time and health dollars at AOC with the hope, and likely the expectation, that the treatment received will result in less knee pain, better mobility, and a significant delay of any joint replacement surgery. I have no doubt that we can do this, but the odds for a great outcome with lasting results will be tilted in your favor, and I believe substantially, if we think of the degenerative arthritis in your affected joints as part of a whole‐body process that comes as we get older – Inflammaging. Briefly, inflammaging is described as a continual low‐grade, whole body inflammation quite common here in the USA where our immune system faces a constant assault from poor diet, obesity, toxins in our air, water, food, radiation, chronic stress, disordered sleep, etc. The result is a higher inflammatory load that accelerates all of the degenerative diseases associated with aging, including osteoarthritis. So, to illustrate, imagine your body as a large, lush, green, thriving tropical rain forest. Now imagine your arthritic knee is a small section of this forest and it is on fire. Because the fire is isolated and the surrounding areas are lush and healthy, we will send one fire bomber (our injection treatments) to drop its fire retardant. It successfully stops the damage allowing the small section to recover. Now, imagine that same small section is ablaze, but now the surrounding forest is dry due to drought and there are some evil arsonists continually starting up little fires in the surrounding areas. That fire bomber will again douse the targeted flames, but the new fires are continually tossing burning embers back into that section, never giving it a full chance to be green, healthy, useful again. Your whole‐body inflammatory load is the arsonist of the story. As the medical director at AOC, I hope you will be open to addressing the systemic inflammation working against your best possible outcome. Lifestyle modifications (diet, exercise, sleep, stress coping) will be discussed here at the office and educational materials provided. We will also carry a number of supplement products known to address inflammaging directly and indirectly. Some have shown direct benefit vs osteoarthritis specifically. Some of these have been found in controlled studies to be as effective vs pain as medicines prescribed for similar reasons, but without the serious side effects. I will be happy to make specific recommendations on an individual basis as part of your care and out of our dedication to providing you the best treatment outcome possible. LRK

Turmeric is that wonderful orange fleshed root that gives flavor and aroma to curry dishes. Curcumin is the active compound in turmeric that is responsible for the brilliant color and its incredible array of health benefits. In terms of research evidence, I think Curcumin is a great place to start when looking for a dietary supplement that addresses not only the symptoms of osteoarthritis, but also the pathology. It has become popular and getting heavy play in main stream media and marketing for good reason - It works. In has been shown to reduce pain and improve mobility in animal models. It appears to slow the progression of OA and preserve cartilage by reducing the production of inflammatory cytokines and matrix metalloproteinases from the involved tissues. It appears to be able to delay the onset of osteoarthritis following injury such as a meniscal or cruciate ligament tear. If what it can do for your knees (and other joints) is not enough to include curcumin in your daily regimen, then here is some added incentive: Besides being anti-inflammatory , which alone helps nearly every organ system in your body, it has significant cancer preventing actions, improves immune function , and even helps protect and improve brain functions including memory! Absorption issues for curcumin have been mostly defeated by the addition of helpful compounds or wrapping the curcumin molecule with another substance that helps pass it through the intestinal lining and into the blood stream. It is well worth paying extra for an absorbable, more bio-active product and will help you avoid any curcumin related GI distress, its most common adverse event. The primary drug interaction to consider is if you are taking any blood thinning medications . It could make you more prone to bleeding and bruising. If you are taking such meds, please discuss taking curcumin with your primary care doctor first as he may want to adjust your medication.